Kuberska, K., Martin, G., Hurst, J. R., & Bafadhel, M. (2025). Respiratory Clinicians’ Views on Offering “Rescue Packs” to Patients Discharged After COPD Exacerbation: Qualitative Interview Study. COPD: Journal of Chronic Obstructive Pulmonary Disease, 22(1). https://doi.org/10.1080/15412555.2025.2524346
What do doctors think about offering “rescue packs” to patients discharged after COPD exacerbation?
Why it matters
Chronic obstructive pulmonary disease (COPD) is a common lung condition affecting over 200 million people worldwide and causing about 3.5 million deaths each year. In the UK, around 3 million people are thought to have COPD, although figures suggest that only around 1 million of those have been formally diagnosed.
People with COPD often experience symptoms like coughing and shortness of breath, which can limit physical activity, and they can be vulnerable to respiratory infections that cause flare-ups of their condition, known as exacerbations. Some of these are severe enough to need hospital care. Some research has shown that if patients start their treatment as soon as they notice a deterioration in their symptoms, with a set of medications called a “rescue pack” that includes antibiotics and steroids, they may be less likely to end up in hospital.
In the UK, these rescue packs are sometimes given through local primary care services or community respiratory teams but getting hold of them in an emergency can be difficult. Some hospitals also give rescue packs to patients when they are discharged after a flare-up. We asked respiratory consultants, registrars and specialist nurses from 20 UK hospitals what they thought about offering rescue packs to patients when they leave the hospital after a COPD flare-up.
What we found
Respiratory clinicians (healthcare professionals specialising in treating people with lung and breathing problems) must make complex decisions about whether to give rescue packs to patients leaving the hospital after a flare-up. While many things can influence this decision, the most important factors for them tend to relate to the individual patient’s situation, not broader concerns like trying to limit overall antibiotic use (antibiotic stewardship).
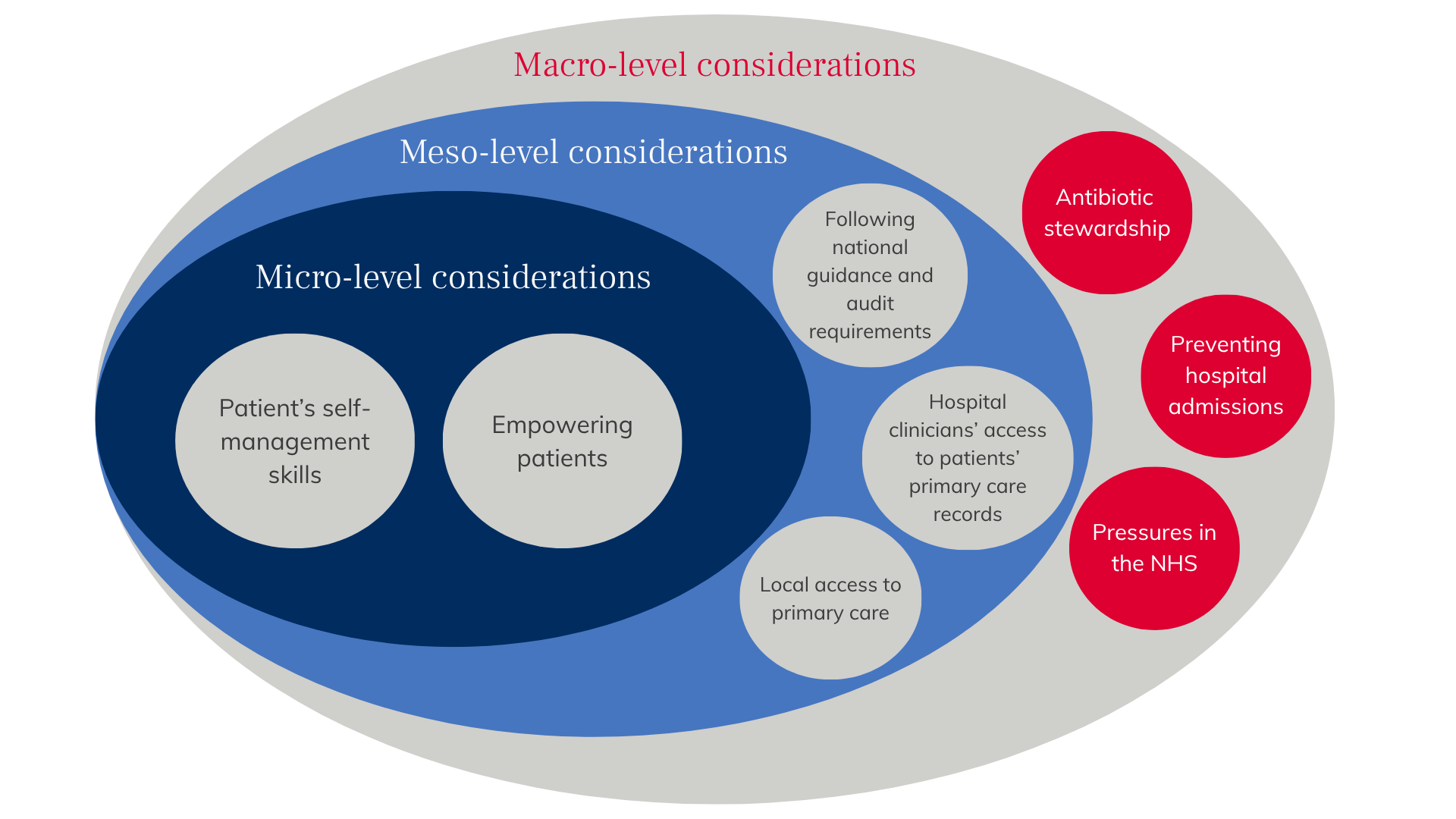
Hospital respiratory clinicians’ views about offering rescue packs to patients when they are discharged from hospital after an exacerbation highlighted an awareness of some of the risks. They agreed that helping patients to manage their COPD on their own was important for effective care. They also spoke about their concerns and recognised the different benefits at three levels: large-scale (macro), organisational (meso), and personal (micro). In the end, despite the difficulty of balancing these often competing concerns, they said that they favoured tailoring decisions to each patient, based on how well they manage their condition and how they’ve used rescue packs in the past.
Although they were aware of large-scale and organisational issues around rescue packs, like the importance of antibiotic stewardship or the lack of access to local GP services, clinicians ultimately focused on what was appropriate for individual patients’ circumstances when they decided whether to give a rescue pack.
The clinicians we interviewed said that some patients need more support than others to make proper use of rescue packs, and recognised that while some people living with COPD know their symptoms well enough to be able to tell symptoms of exacerbation from a “bad day”, others either made too much use of rescue packs (as their prescription records showed) or underused them, arriving at emergency departments in a very poor state. It is important to offer tailored support to patients with COPD to help them decide when or whether to start a rescue pack.
Offering support to patients was often mentioned in the interviews. This is explicitly recommended in guidelines and evidence-based recommendation reports. But what’s less clear is what this support looks like for patients with different needs or preferences, or who live in areas where healthcare isn’t easily available. The clinicians in the study agreed that even if there is strong evidence to show that rescue packs are helpful at discharge, the decision to offer one still needs to be based on each patient’s individual situation, including things like whether they can access community-based services, and whether they’re able to judge when to use the pack, when not to use it, and when to ask for more help.
This study shows there are complex issues around supporting people with COPD and raises questions about how much we can – or should – rely on patients’ self-management.