Waring J., et al. (2023), Implementing a Perioperative care of Older People undergoing Surgery (POPS) service: findings from a multi-site qualitative implementation study. Age and Ageing. https://doi.org/10.1093/ageing/afad149
Implementing a Perioperative care of Older People undergoing Surgery (POPS) service: findings from a multi-site qualitative implementation study
Why it matters
The number of older people having surgery is increasing. However, older patients are more likely to have complications after surgery than younger patients as they often have multiple health conditions and age-related problems such as frailty and a decline in mental ability. These factors increase the risk of surgery and can hinder recovery.
Surgical pre-assessment usually focuses on the patient’s physical fitness for surgery, not the broader range of health-related factors that are important to consider in older patients.
The Perioperative care for Older People undergoing Surgery (POPS) model was developed to provide a holistic assessment of an older person’s medical, physiological and functional condition prior to surgery. The assessment is then used to inform interventions that can reduce the risk of complications.
The POPS model is increasingly being implemented across the English and Welsh NHS, but there are often challenges in introducing these new ways of providing care that need to be better understood.
Approach
This independent study, led by THIS Institute Fellow Professor Justin Waring, outlines the key activities and strategies that are needed for the POPS model to be successfully implemented and become part of routine practice in a hospital.
The research involved case studies in six NHS hospitals that have implemented the POPS model and interviews with the people involved, including consultant geriatricians, surgeons, anaesthetists and nurses. Previous research on the implementation of the POPS model has focused on a single hospital site. This research provides further evidence about the strategies and activities used by clinical leaders to implement the POPS model, with the aim of producing recommendations for other hospitals that are looking to do the same.
Findings
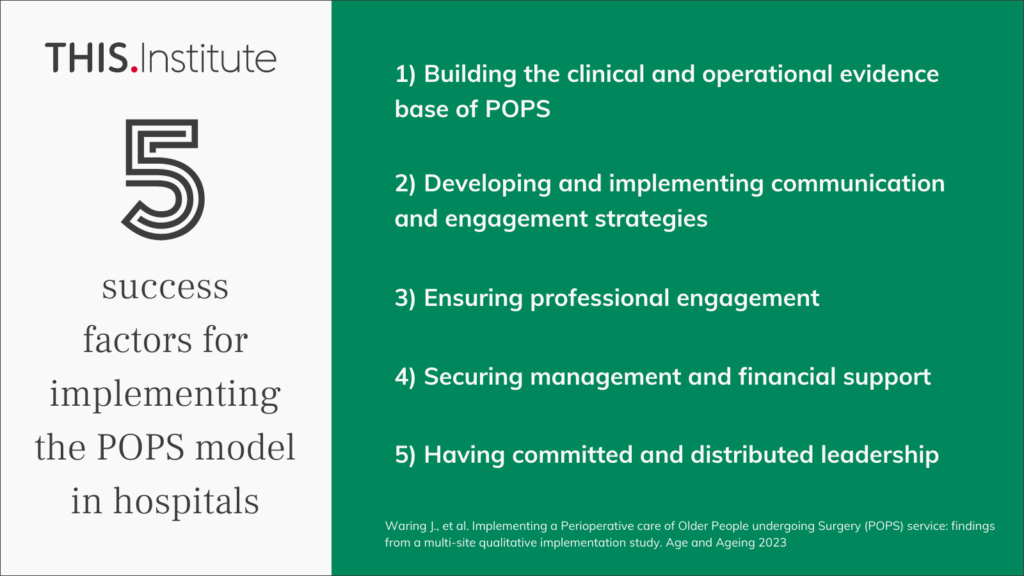
The main barriers to the introduction of the POPS model in the six case study sites were limited managerial and financial support for the allocation of clinical time, and apprehension among some surgeons and anaesthetists about the impact of the model on established ways of working.
These barriers were addressed by the clinical leads for the POPS model in each hospital through a series of connected activities. To secure management and financial support, POPS was often introduced as a pilot in one surgical pathway and this made it possible to demonstrate the clinical and operational benefits of the model.
To encourage professional engagement, it was found to be essential to provide surgeons and anaesthetists with relevant information about how the POPS model could be integrated into surgical pathways without significant disruption and to further demonstrate its clinical value.
To address the concerns of management and clinicians, the implementation of POPS required the ongoing building of evidence to demonstrate the clinical and operational benefits of the approach. This included clinical research evidence, local service level data, and improvement in performance in external audits or registries. It also required POPS leaders to build collaborative relationships and to encourage other professionals to champion the model and to extend it to other surgical pathways. Finally, having leaders who were committed to implementing the POPS model was vital, as they ensured activities were coordinated and promoted.
This paper provides learning from early adopters of the POPS model and recommendations for successful implementation.