Martin, G., Chew, S., McCarthy, I., Dawson, J., Dixon-Woods, M. (2022), Encouraging openness in health care: Policy and practice implications of a mixed-methods study in the English National Health Service, Journal of Health Services Research & Policy. doi: 10.1177/13558196221109053.
Encouraging openness in health care: Policy and practice implications of a mixed-methods study in the English National Health Service
Why it matters
Openness is vital in ensuring everyone involved in healthcare delivery feels able to voice concerns about problems of quality and safety. However, delivering a culture of openness has often proved challenging.
The failings at Stafford Hospital in the 2000s led to extensive policy interventions to promote openness, transparency and candour in the NHS. But subsequent scandals show that there are still deficits in openness.
We carried out a large mixed-methods evaluation programme to examine organisational responses to national policies aimed at increasing openness.
Approach
We evaluated the implementation of policies introduced following government-commissioned reports on poor quality of care and failings of openness in the English NHS.
The study involved four sub-studies: analysis of data from surveys of NHS staff and service users; interviews with senior stakeholders in NHS provider organisations and the wider system; a survey of board members of NHS provider organisations; and case studies of six NHS organisations.
The case studies looked to find out whether provider organisations’ efforts to increase openness resulted in real changes in staff values, attitudes and actions at the sharp end of care, and in patients’ opportunities and experiences around openness – and what features contribute to success. In these case studies, we focused on three policies: the Duty of Candour, the introduction of Freedom to Speak up Guardians, and changes to processes for investigating serious incidents.
What we found
Our findings indicate a mixed picture of progress towards improving openness in the NHS. There is little to suggest that the significant shifts in culture around openness sought by policy-makers have been consistently achieved.
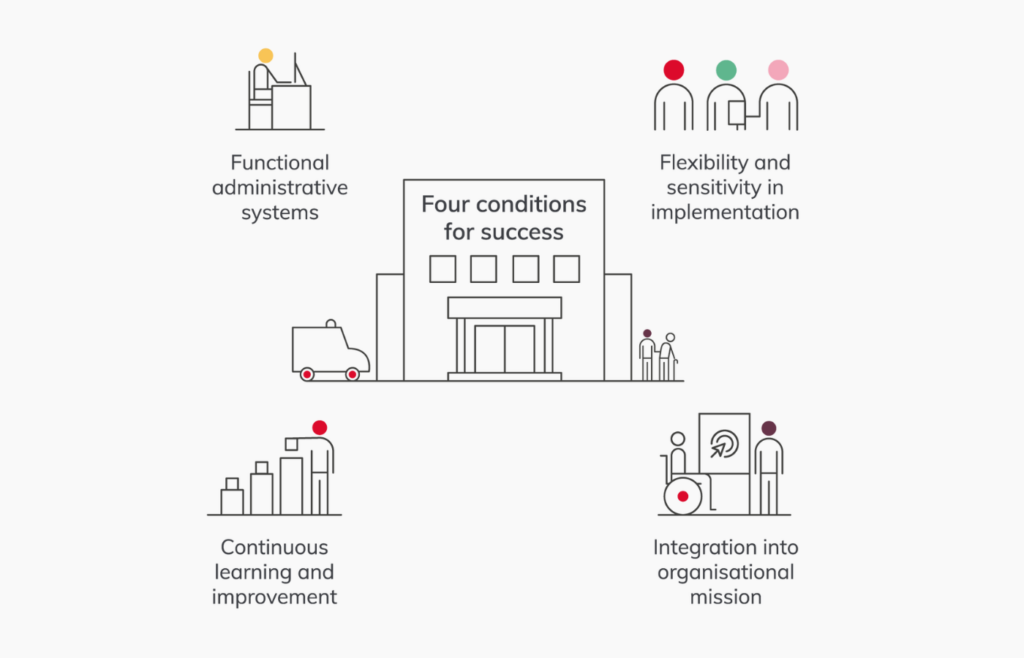
We identified four conditions necessary for sustained progress in improving openness:
- Openness needs to be an organisational priority that is integrated into the core organisational mission: Organisations where openness appeared to be a ‘bolt-on’, an optional extra or a temporary fixation invested less effort in improving openness, and it was often clear to staff that their work was superficial.
- Administrative systems need to be functional and effective: A well-functioning infrastructure can make a big difference to organisations’ ability to identify problems, share learning and monitor progress towards improvement.
- Systems and processes must be flexible and sensitive: Following a standard approach for every issue can have unintended negative consequences, especially for sensitive issues; adjusting processes, timescales and approaches to interaction can help them to run smoothly, and account for the preferences of those involved.
- There must be an organisational ethic of continuous inquiry, learning and improvement: Viewing openness as a time-limited project is unlikely to result in sustainable improvement; trying things out, reflecting on what worked, and using learning to inform further work on an ongoing basis is crucial.
We also identified four challenges that hamper progress towards openness:
- A reliance on goodwill and discretionary effort: Workforce pressures in the NHS are large for many groups of staff, and much openness activity relies on adding to the workloads of these groups.
- Caring for staff, patients and relatives who seek openness: Those involved in patient safety incidents and in raising concerns about quality and safety face significant emotional stress; support for them is crucial.
- The limits of values-driven approaches: Organisations may align their work around openness with the values and interests of their staff, and this approach has much merit; but organisations also need to make clear the standards they expect of their staff, and the means of enforcing those standards.
- The continued marginality of patients, carers and families: Most policy activity around openness casts patients and families as passive beneficiaries of interventions, but they offer an important source of insight for improvement.
Variation in policy implementation offers important lessons on how organisations can better deliver openness, transparency and candour. Our study demonstrates the importance of going beyond simple implementation of national policy and reveals the difference that nuanced approaches to policy translation can make.