Leading a career in clinical academia that places the patient first


For patients who survive a critical illness, being discharged from the hospital is sometimes only the beginning of their journey. Patients and their families can have long-term issues related to the critical illness – around 25% of ICU survivors end up being readmitted to hospital within three months of discharge. Despite efforts to reduce this number, there is limited evidence offering potential solutions. With studies more commonly exploring the impact on admissions hospital – THIS Fellow and Professor of Nursing, Jo McPeake’s research focuses on how we can improve health outcomes for patients and family following acute illness.
Putting the patient first
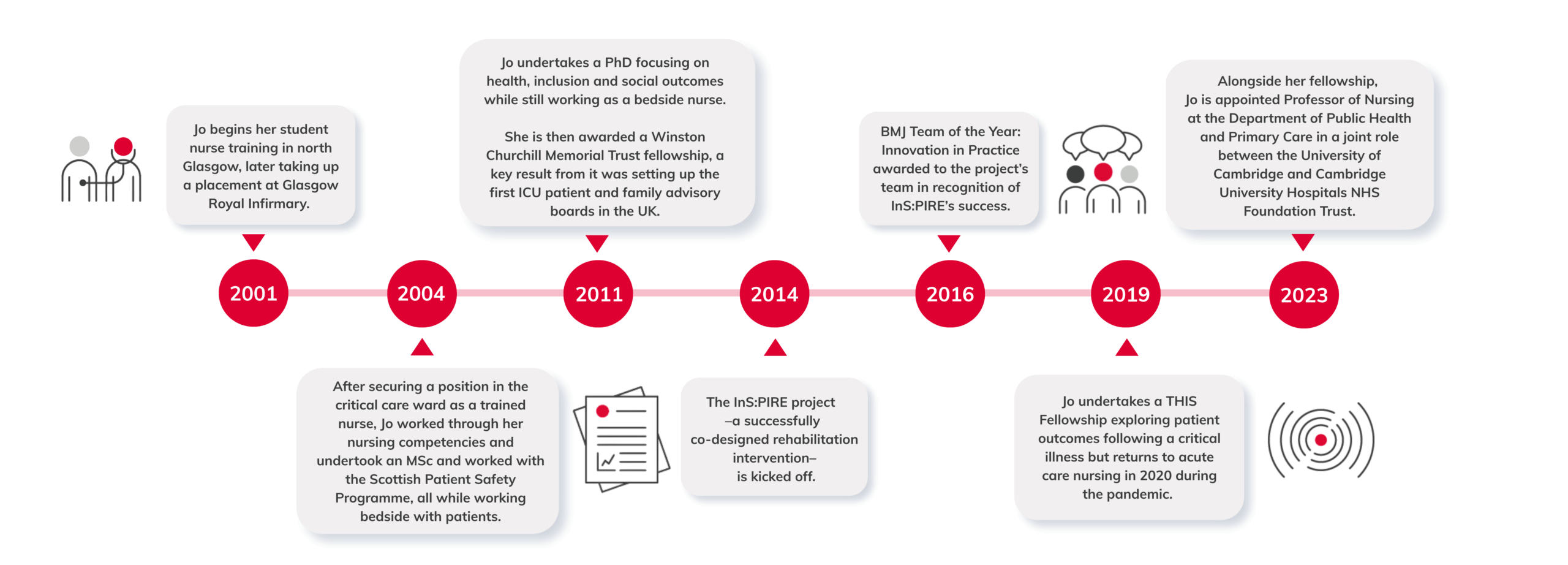
Jo began her career as a student nurse in Glasgow and it was during her clinical placement that she saw how social inequalities impacted health and access to care.
She carried on her training at Glasgow Royal Infirmary, where she learned the importance of exceptional communication and teamwork. Above all, she began to appreciate the important role that family and carers played, including their relationship with clinical teams, in determining and improving the health outcomes of patients.
One of Jo’s final training placements was in the intensive care unit where she grew to love the type of nursing that is required when working in a busy critical care ward. Following her placement in intensive care, Jo went on to secure a permanent position on the ward.
While she was working in critical care, Jo developed her nursing competencies (a formal requirement for nurses) alongside academic research. During this time, she noticed the impact that improvement research was having on safety processes and patient outcomes, for example with the ongoing work of the Scottish Patient Safety programme in critical care units in Scotland which motivated her to continue her research journey.
Bringing research to the front line of hospital work
Jo undertook a PhD which focussed on health inclusion, exploring alcohol related admissions in critical care, specifically understanding what happened to patients when they were discharged. She then applied successfully for a Winston Churchill Memorial Trust fellowship, which gave her the opportunity to travel and work in different hospitals in the United States.
She took the learning from this fellowship and used it to set up one of the first Intensive Care Unit (ICU) patient and family advisory boards in the UK, co-designing interventions to support patient outcomes and advocating for caregivers. She led the InS:PIRE project: a successful five-week recovery programme that focused on patient education, peer support and helping people take control of their own recovery. The project was a notable success, with the Glasgow Royal Infirmary team winning BMJ Team of the Year award 2016 for Innovation into Practice.
Jo felt there was much more that needed to be done because despite the support InS:PIRE introduced to patients and caregivers, many critical care patients ended up back in hospital following discharge.
To understand why this was happening and what could be done about it, she applied for a THIS Institute fellowship in 2019. The fellowship encouraged Jo to work closely with patients and collaborators to co-design solutions and provided her with a tailored leadership programme which was designed to help her optimise her research.
From a patient perspective, when people are recovering, the last thing they want is to return to hospital.
Improving health and social care
Jo focused on the use of unscheduled care following critical illness and set out to understand drivers for hospital readmissions following a serious illness. Her fellowship brought together health and social care services and was developed in close collaboration with patients and public involvement (PPI) groups, using a range of innovative methodologies and data sources.
At the start of the pandemic in 2020, Jo returned to critical care nursing on and off for two years to support patients during this turbulent time. She also continued to be part of various health inclusion research projects, some of which looked at outcomes of critical illness at a national level.
Following the pandemic, Jo returned to her THIS fellowship, working with experts from multidisciplinary fields to find practical solutions to the problem she was studying. In 2023 Jo was appointed Professor of Nursing at the Department of Public Health and Primary Care and for Cambridge University Hospitals NHS Foundation Trust, a key role in generating evidence to improve quality and safety in healthcare and building research capacity. Jo is responsible for an exciting and high impact programme of research, with a particular focus on health inequalities and critical care. She also covers education modules and supports the academic training and development of nurses, midwives and allied health professionals.
At the end of her fellowship project, we asked Jo to share her insights. She said her research led her to rethink some of the challenges people face after a critical illness, when looking at hospital readmissions as an outcome for success (in interventional programmes across critical care and long-term conditions.) She shared: “From a patient perspective, when people are recovering, the last thing they want is to return to hospital.” But in interviews with those who were re-admitted to hospital, Jo found that if people become ill again, priorities and needs change, and our system must adapt to this. She also found that patients’ needs change during the recovery or progression of illness, so the research being conducted needed to be dynamic to recognise these changes.
When reflecting on her experience and its impact on her career trajectory, Jo shared that her fellowship provided her with flexibility and support, giving her the skills, confidence and experience which facilitated her roles in NHS management and as Professor of Nursing. This approach also enabled Jo to support COVID-19 related research where she created lasting relationships, collaborations and ongoing research – and most importantly, improvements to patient care in the NHS.
Learn more about Jo’s research fellowship and watch her inaugural lecture as Professor of Nursing here.