Specialty COPD care during COVID-19: perspectives on remote delivery

Background
Chronic obstructive pulmonary disease (COPD) is a term used to describe several lung conditions that make breathing difficult. In the UK, around 1.2 million people have a COPD diagnosis.
In 2020, to reduce the risk of spreading COVID-19, the NHS moved quickly to reduce the number of face-to-face appointments for people with long-term conditions. Some COPD services adapted rapidly to provide remote care for people with COPD via phone and video appointments or other forms of remote care.
For all conditions, there are advantages and disadvantages to providing remote care. Some people with COPD are clinically extremely vulnerable and changes or limitations to care may cause difficulties. This study sought to provide insights into the move towards remote delivery of care during the COVID-19 pandemic. We also wanted to identify agreement and disagreement among people with COPD and their clinicians about which aspects of COPD care can most appropriately be delivered remotely.
Our approach
The study, supported by the Royal College of Physicians, asked which aspects of routine specialist COPD care can and cannot be delivered using remote communication.
It took place over two stages, informed by a rapid literature review. The study was conducted using the Thiscovery online research platform.
First, questionnaires were developed about the experience of remote care for clinicians providing specialist COPD care and people with COPD. The questionnaires were similar, but clinicians were asked extra questions about support for remote care in their organisations.
Second, a consensus-building process was undertaken in which participants in the study (people with COPD and clinicians) were asked to rate the appropriateness of delivering different aspects of COPD care remotely. These aspects of care were defined based on NICE standards for care of people with COPD. We also asked participants what should be prioritised in improving remote care for COPD.
Altogether, 55 clinicians and 19 people with COPD completed the survey; 23 clinicians and 20 people with COPD took part in the consensus-building process.
What we found
It was clear that remote COPD care had become widespread since the start of the pandemic, with 95% of clinicians reporting that they were providing remote alternatives to face-to-face care, mainly by phone and/or video.
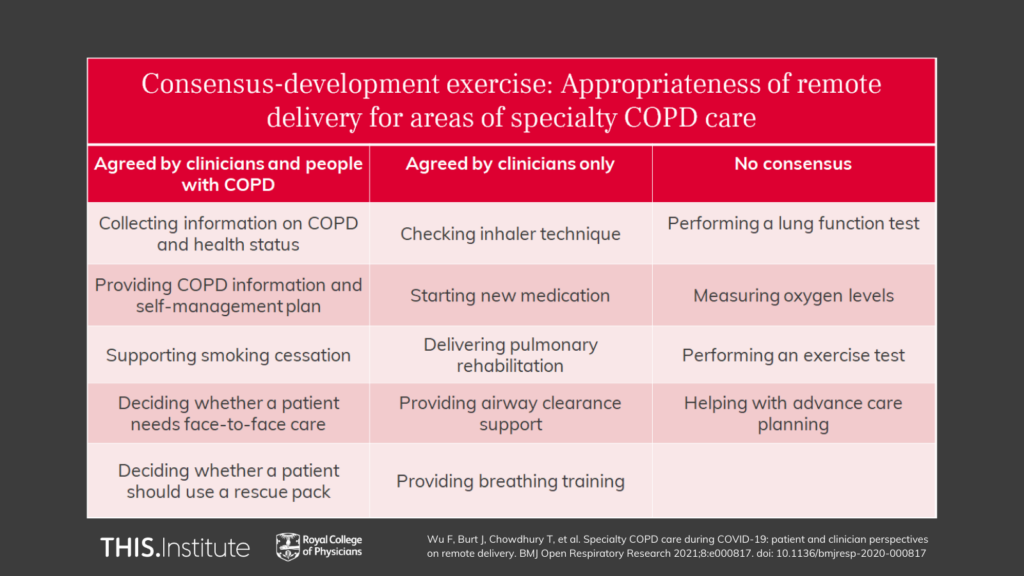
Participants reported that many aspects of remote care worked well, but both people with COPD and clinicians reported limitations. In some areas there was consensus between people with COPD and clinicians, but it is interesting to note that in other areas no consensus was reached.
There was consensus that five areas of specialist COPD care can be delivered well remotely:
- Collecting information on COPD and health status
- Providing COPD information and self-management plan
- Supporting smoking cessation
- Deciding whether someone needs face-to-face care
- Deciding whether someone should use a rescue pack.
For five areas of care, clinicians reached consensus on appropriateness but people with COPD did not:
- Checking inhaler technique
- Starting new medication
- Delivering pulmonary rehabilitation
- Providing airway clearance support
- Providing breathing training.
For the remaining areas, there was no consensus on appropriateness (but neither was there consensus that remote care was not appropriate):
- Performing a lung function test
- Measuring oxygen levels
- Performing an exercise test
- Helping with advance care planning.
For some of these areas, services may wish to consider whether limited face-to-face contact is still needed to deliver care.
By finding out what works well for remote COPD care now, we can help to ensure that people with COPD and clinicians can benefit from improved care beyond the pandemic, through continued remote care for symptoms assessment, support to stop smoking and signposting to other services.
At a glance