Framework publication: Wanyonyi-Kay, K., Martin, G., Ball, S., Cunnington, P., Boney, O., Moonesinghe, S. R., Dixon-Woods, M. & The Perioperative Expert Contributor Group. 2025. A quality framework for perioperative care: rapid review and participatory exercise. medRxiv, https://doi.org/10.1101/2025.08.13.25333583
Developing a framework and core indicators for measuring good quality perioperative care
Nearly 10 million people have surgery in the UK each year, making it vital to monitor the quality of care they receive before, during and after their operation. To understand care quality, three key aspects of surgery are important: First, “structure” indicators look at aspects of healthcare organisation and structure, such as having the right number of staff and correct equipment in place. Second, “process” indicators look at actions taken during the course of caring for patients – such as providing pain management after the operation. Finally, “outcome” indicators assess how well the patient is doing following surgery, looking at things such as mobility and range of function.
There is no shortage of indicators for monitoring surgical care – many hundreds have been published or used. But they aren’t all well-supported by evidence, and few include input from patients and healthcare staff. We wanted to develop an evidence-based framework of the key aspects of structure and process important to quality, and to identify a set of indicators that reflect good care. We were committed to working with patients, carers and healthcare professionals so that the framework would reflect what was important to them.
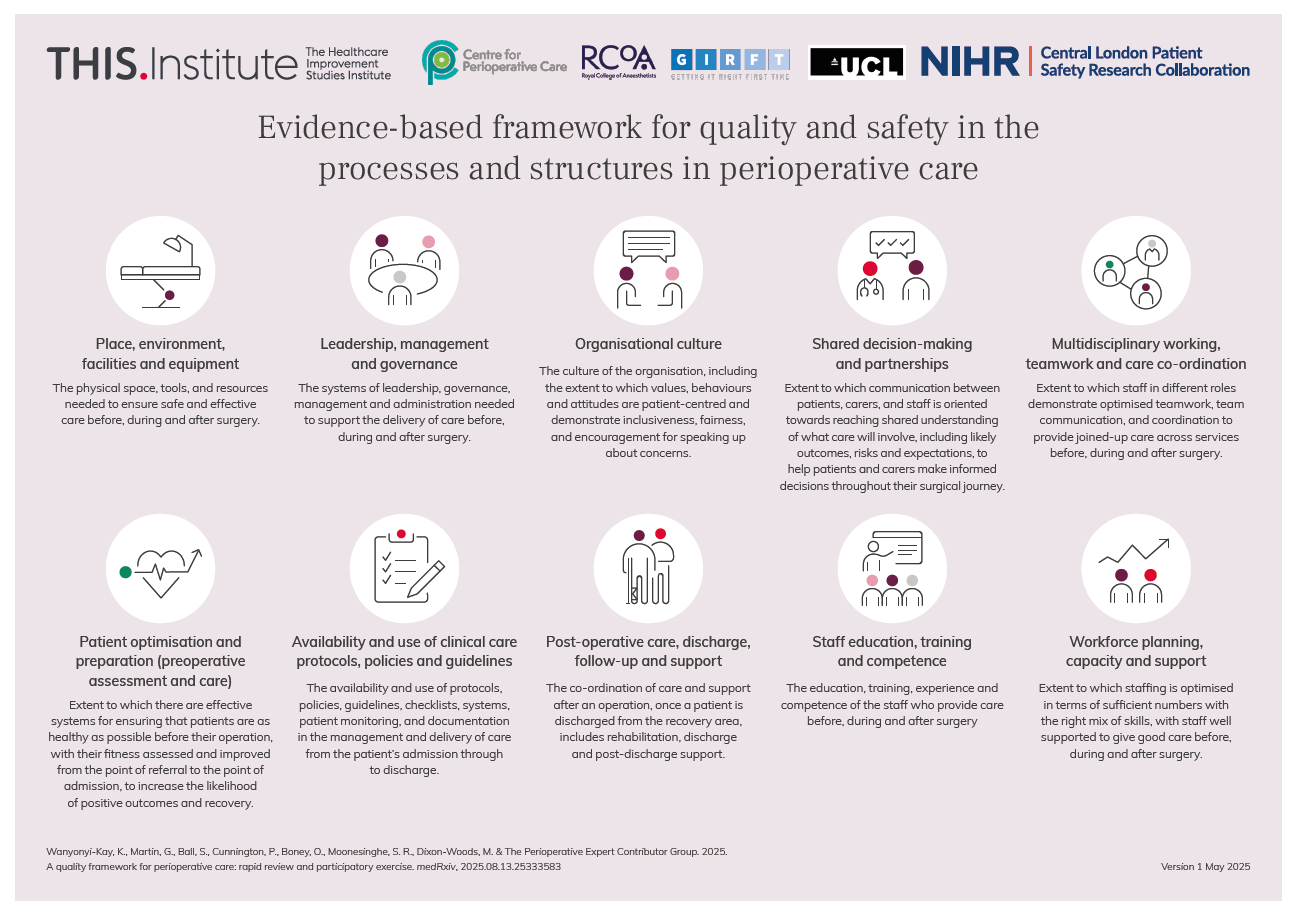
We reviewed the available literature as a first step. We then shared our findings with a small group of patients, carers, healthcare professionals, and managers. They helped us to identify 10 major categories that could be used to classify perioperative structure and process indicators, which were:
- place, environment, facilities and equipment
- leadership, management and governance
- organisational culture
- shared decision-making and partnerships
- multidisciplinary working, teamwork and care co-ordination
- patient optimisation and preparation (preoperative assessment and care)
- availability and use of clinical care protocols, policies and guidelines
- care after surgery, discharge, follow-up and support
- staff education, training and competence
- workforce planning, capacity and support
We used these categories to organise over 600 indicators – ranging from preparing patients well for surgery to supporting patients and carers to make informed decisions. Then, with the help of more than 250 patients and professionals, and following intensive workshops, we identified which were the most important indicators within each category.
The final framework, with its 10 categories and 28 core indicators, will be valuable for monitoring quality of care, helping to show where care is good and where improvement can be targeted.
Click the image to view in fullscreen.
Place, environment, facilities and equipment
The physical space, tools, and resources needed to ensure safe and effective care before, during and after surgery.
Structure indicators
- Availability of suitable spaces for private conversations to support patients to make an informed decision about consent to surgery (Core indicator)
- Availability of ring-fenced Critical Care beds for elective surgical patients (Core indicator)
- Availability of a senior doctor or decision maker (e.g., consultant or Specialty and Specialist (SAS)) at the hospital within 30 minutes (Desirable)
- Availability of equipment and relevant consumables for patient-controlled pain relief (Desirable)
Process indicators
- Proportion of cases where routine checks of all anaethesia equipement before use are conducted and documented according to national safety guidelines (Core indicator)
- Proportion of surgery patients who spend their hospital stay on a surgical ward or high care beds (Desirable)
Leadership, management and governance
The systems of leadership, governance, management and administration used to support the delivery of care before, during and after surgery.
Structure indicators
- Perioperative pathways in place that follow National Confidential Enquiry into Patient Outcome and Death recommendations, including prioritisation based on urgency of surgery (Core indicator)
- Systems in place for reporting, investigating and learning from serious incidents and near misses (Core indicator)
Process indicators
- Proportion of scheduled elective operations cancelled within 72 hours of surgery (Core indicator)
- Frequency (per month) of multidisciplinary Mortality and Morbidity meetings (Core indicator)
- Whether data are submitted reliably to national audit programmes and relevant results shared with the local team (Desirable)
- Proportion of high risk patients (predicted risk of death >5%) where a senior (consultant/SAS) surgeon and senior (consultant/SAS) anaesthetist are both present in theatre (Desirable)
Organisational culture
The culture of the organisation, including the extent to which values, behaviours and attitudes are patient-centred and demonstrate inclusiveness, fairness,
and encouragement for speaking up about concerns.
Structure indicators
- Confidential and safe systems in place for staff to speak up about concerns (Core indicator)
- Systems in place to enable dedicated time for team briefings within staff schedules (Core indicator)
- Systems in place for collecting and sharing NHS staff and patient survey results and GMC national training survey results (Desirable)
Process indicators
- Proportion of patient-reported outcomes routinely recorded (Core indicator)
- Proportion of patient complaints and concerns investigated and analysed to identify areas for improvement (Core indicator)
- Proportion of patients who report concerns, complaints and harm (Desirable)
Shared decision-making and partnership in care
Extent to which communication between patients, carers, and staff is oriented towards reaching shared understanding of what care will involve, including likely outcomes, risks and expectations, to help patients and carers make informed decisions throughout their surgical journey.
Structure indicators
- Systems in place to support family and caregivers to be involved in making decisions (Core indicator)
- Systems in place for making reasonable adjustments to support patients’ and their caregivers’ with specific communication and decision-making needs (e.g. lacking or fluctuating capacity, language barriers, accessibility, cultural) (Desirable)
- System in place for surgery patients to seek clinical advice after hospital discharge following surgery including out of hours and weekends (Desirable)
Process indicators
- Proportion of patients that have a documented shared decision-making consultation to decide whether surgery is the preferred option including a discussion of risks, benefits and alternative options (Desirable)
- Proportion of cases where the medical or nursing team updates the patient’s family/ caregivers on the outcome of the surgery immediately after surgery (Desirable)
Multidisciplinary working & care co-ordination
Extent to which staff in different roles demonstrate optimised teamwork, communication, and coordination to provide joined-up care across services before, during and after surgery.
Structure indicators
- Availability of a multidisciplinary team to support post-operative recovery and safe discharge planning (Core indicator)
- Availability of multidisciplinary team to support a patient to prepare for their surgical admission (Desirable)
Process indicators
- Proportion of patients referred from primary care and/or community-based services for elective surgery with key information missing such as about their long term conditions (Core indicator)
- Proportion of complex frail and/or older patients who are reviewed before and after surgery by a specialist team (e.g., orthogeriatrician-led team or Perioperative Medicine for Older People undergoing Surgery (POPS) team) (Desirable)
- Proportion of patients with documented handovers between transitions of care across the perioperative journey (Desirable)
- Proportion of patients whose care decisions before, during, and after surgery are made by specialist multidisciplinary teams (Desirable)
Preoperative assessment and care
Extent to which there are effective systems for ensuring that patients are as healthy as possible before their operation, with their fitness assessed and improved from the point of referral to the point of admission, to increase the likelihood of positive outcomes and recovery.
Structure indicators
- Systems in place to ensure patients receive appropriately tailored pre-operative testing as per national guidelines (Core indicator)
- A system or hospital policy in place that aims for all tests and investigations before surgery to be done during a single hospital visit (Core indicator)
- Systems in place to ensure patients are advised and/or enabled to have a shower, bath or bed bath on the day of surgery/the day before (Desirable)
Process indicators
- Proportion of elective surgical patients who receive preoperative assessment before they are given a date for their surgery (Core indicator)
- Proportion of major elective surgical patients screened for frailty, anaemia, diabetes, and hypertension (and treated where needed) (Core indicator)
- Proportion of elective surgical patients who have a documented pre-operative risk assessment score (Desirable)
- Proportion of elective surgical patients whose surgery is delayed at pre-assessment (Desirable)
Clinical care protocols, policies and guidelines
Extent to which protocols, systems, good practice in documentation and patient monitoring policies, guidelines and checklists are available and used from the patient’s admission through to discharge.
Structure indicators
- Guidelines and/or policies in place for managing perioperative delirium, confusion and/or agitation (Core indicator)
- Guidelines and/or policies in place for managing perioperative anaemia (Core indicator)
- Guidelines and/or policies in place for managing perioperative pain, including 24/7 availability of a service and trained staff for managing severe pain (Core indicator)
- Criteria in place for discharge from post-anaesthetic recovery area (Desirable)
- System in place for booking elective critical care bed (Desirable)
Process indicators
- Proportion of surgeries with WHO surgical checklists completed and documented in the operating theatre (Core indicator)
- Proportion of patients assessed by an anaesthetist on the day of their surgery (Core indicator)
- Measure of patients’ undergoing major surgery whose blood loss is measured and recorded during surgery (Desirable)
- Proportion of major elective surgeries following Enhanced Recovery After Surgery (ERAS) protocol or pathway after surgery (Desirable)
- Proportion of patients’ whose nutritional status is recorded before major elective surgery (and any issues are escalated for further advice if needed) (Desirable)
Post-operative care, discharge, follow-up and support
The co-ordination of care and support after an operation, once a patient is discharged from the recovery area, including rehabilitation, discharge and post-discharge support.
Structure indicators
- Systems in place for providing follow-up within 30 days of going home from hospital, rehabilitation and/or appropriate support at home after discharge (Core indicator)
Process indicators
- Proportion of patients and caregivers who receive advice about medications, caring for their wound / dressing and rehabilitation (where applicable) after hospital discharge (Core indicator)
- Proportion of patients with unplanned admission to Critical Care ward after surgery (Desirable)
- Proportion of patients whose mobility and ability to self-care are assessed before hospital discharge (Desirable)
Staff education, training, and competence
The education, training, experience and competence of the staff who provide care before, during and after surgery.
Structure indicators
- System in place for continuing professional development of staff and ensuring compliance with mandatory training, including interprofessional training (Desirable)
- System in place for providing staff training on using new and existing equipment, following clincial care guidelines (Desirable)
Process indicators
- Proportion of staff in the post-anaesthesia care unit (the area for recovery after surgery) who are trained to the required standard (Core indicator)
Workforce planning, capacity and support
Extent to which staffing is optimised in terms of sufficient numbers with the right mix of skills, and staff well supported to give good care before, during and after surgery.
Structure indicators
- Schedules are used showing where and when staff should meet to hand over responsibility for the patient, as well as who needs to be there for the hand over (Core indicator)
Process indicators
- Proportion of emergency surgery cases admitted to the intensive care unit that are reviewed by a senior doctor (consultant/SAS) in intensive care medicine within 12 hours (Core indicator)
- Proportion of patients whose move from the recovery area is managed by two members of staff, with at least one staff member being fully trained (Desirable)